Translate this page into:
A Study Comparing the Results of Diathermy Versus Scalpel for Inguinal Skin Incisions
*Corresponding author: H. M. Abhijith, Department of General Surgery, Gulbarga Institute of Medical Sciences, Kalaburgi, India abhijithhiremath@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abhijith H. M, & Shafiuddin M. A Study Comparing the Results of Diathermy Versus Scalpel for Inguinal Skin Incisions. Karnataka J Surg. 2025;2:6–10. doi: 10.25259/KJS_15_2024
Abstract
Objectives
The advent of electrocautery has introduced a significant alternative to traditional scalpels for making skin incisions in surgical procedures. Electrosurgery, also known as surgical diathermy, involves passing high-frequency electric current through body tissues to achieve coagulation, fulguration, and cutting. There are two main types of diathermy: monopolar, where the current travels from an electrode near the target tissue to a fixed electrode elsewhere on the body, and bipolar, where both electrodes are on a single device, allowing the current to flow through the treated tissue alone. Despite the advantages of diathermy, including reduced bleeding and quicker incision time, concerns about wound infection, delayed healing, and scarring have limited its use for skin incisions.
Material and Methods
This study aims to compare the outcomes of diathermy versus scalpel incisions in terms of incision time, blood loss, postoperative pain, wound infection, and scar characteristics in inguinal surgeries. Conducted at Gulbarga Institute of Medical Sciences, Kalaburgi, this prospective randomised control study spanned from August 2023 to May 2024. A total of 81 patients were randomly assigned to either the scalpel incision group [n = 40] or the diathermy incision group [n = 41].
Results
The findings indicate that diathermy incisions offer significant benefits over scalpel incisions, including reduced incision time, lower blood loss, and decreased postoperative pain. The study utilised the Manchester Scar Score to assess wound characteristics, finding no significant difference between the two groups in terms of wound healing and scar quality. The safety and efficacy of electrocautery were further supported by the absence of significant differences in postoperative wound complications, hospital stay duration, and cosmetic outcomes between the two methods.
Conclusion
In conclusion, diathermy presents a safe and effective alternative to scalpel incisions, offering reduced intraoperative blood loss and postoperative pain without compromising wound healing or increasing complications. However, the choice between diathermy and scalpel should consider the surgeon’s expertise and the specific surgical context. While diathermy shows clear advantages, certain scenarios may still necessitate the use of a scalpel. Thus, the optimal surgical approach should be determined through careful evaluation of each individual case.
Keywords
Blood loss
Diathermy
Electrocautery
Electrosurgery
Operative
Postoperative pain
Randomised controlled trial
Scars
Skin incisions
Surgical
Surgical procedures
Wound healing
Wound infection
INTRODUCTION
Traditionally, scalpels have been the standard tool for making skin incisions. However, since the advent of electrocautery, it has gained popularity for tasks like coagulation and cutting. Electrosurgery involves the use of high-frequency electric current to achieve specific clinical outcomes, and the term “diathermy” is derived from the Greek words “therma” (heat) and “dia” (through), meaning “heating through tissues.” Carl France Nagelschmidt, a German physician, first coined the term in 1909.[1–3]
Electrosurgery, also referred to as surgical diathermy or electrocautery, is widely used in surgical procedures for coagulation, fulguration, and cutting. There are two main types of diathermy: monopolar and bipolar. In monopolar diathermy, the electrical current flows from one electrode near the target tissue to a separate electrode placed elsewhere on the body, usually near the leg or buttocks. In contrast, bipolar diathermy uses both electrodes on a single device, with the current passing only through the tissue being treated, minimising the risk to surrounding tissues.[4,5]
While scalpels are commonly used for skin incisions, they often lead to bleeding that can obstruct the surgical field. Diathermy offers an alternative, primarily used for tissue destruction and hemostasis. However, surgeons often avoid diathermy for skin incisions due to concerns about wound infection, delayed healing, and scarring.[6–8] This study aims to compare the effectiveness of diathermy and scalpel incisions in terms of incision time, blood loss, wound characteristics, and scar assessment in abdominal surgeries at a tertiary care hospital in Gulbarga.
Aim and objectives
The aim of this study is to compare the outcomes of inguinal incisions versus scalpel incisions in both elective and emergency operations, focusing on incision time, incisional blood loss, postoperative pain, postoperative wound infection, and scar characteristics.
Selection of study subjects
Simple randomisation – Chit based
Sample size
Sample collected [N] = 81 [Table 1].
Inclusion criteria
Patients undergoing elective surgery for whom an inguinal incision is taken.
Patients aged 18–65 years.
Patients on anticoagulants, known cases of coagulopathies.
Exclusion criteria
Patients aged <18 years and >65 years.
Scar at planned incision site.
Patients with pacemakers.
Patients with preexisting pain at the incision site or any neuropathy.
Immunocompromised patients due to chemotherapy, immunosuppressants, corticosteroids, etc.
Pregnancy.
Data collection
Data regarding history, clinical examination, nature of surgery, and postoperative outcome will be included
MATERIAL AND METHODS
A total of 81 patients were included in the study, divided equally into two groups: Group A (40 patients) underwent scalpel incisions and Group B (41 patients) underwent diathermy incisions [Table 2 and Figure 1]. Both groups were operated on by the same surgical unit. Patients were informed about the benefits and risks of each incision method, and consent was obtained. All surgeries were performed under spinal anaesthesia, with a standard antibiotic protocol using Inj. Ceftriaxone [Table 3 and 4].
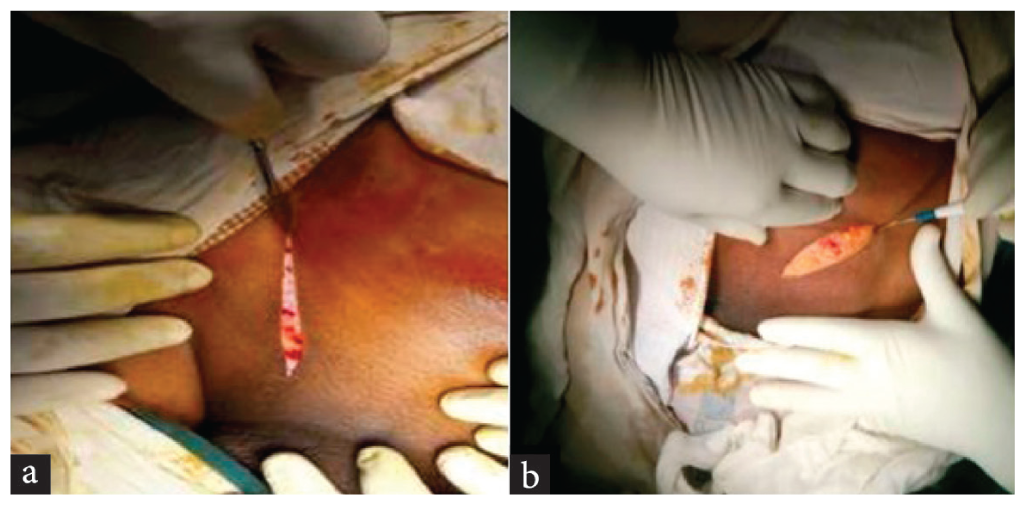
- a) Operative incision with scalpel, b) Operative incision with diathermy.
Randomisation was done using a chit system. In the scalpel group, incisions were made with a no. 22 scalpel blade, with haemostasis achieved by applying pressure with a sterile swab. Diathermy was only used for deeper incisions. In the diathermy group, a monopolar diathermy pencil was used at a 20 CUT mode with 434 KHz [Figure 2 and 3]. Blood loss during the incision was measured by weighing sterile swabs pre- and post-incision, and incision time was recorded with a stopwatch [Table 5]. Postoperative pain was managed with Inj. Diclofenac and, if needed, Inj. Tramadol and assessed using a visual analogue scale (VAS). Wounds were evaluated using the South Hampton wound scoring system on days 4, 10, and 28 [Table 6, 7 and 8].
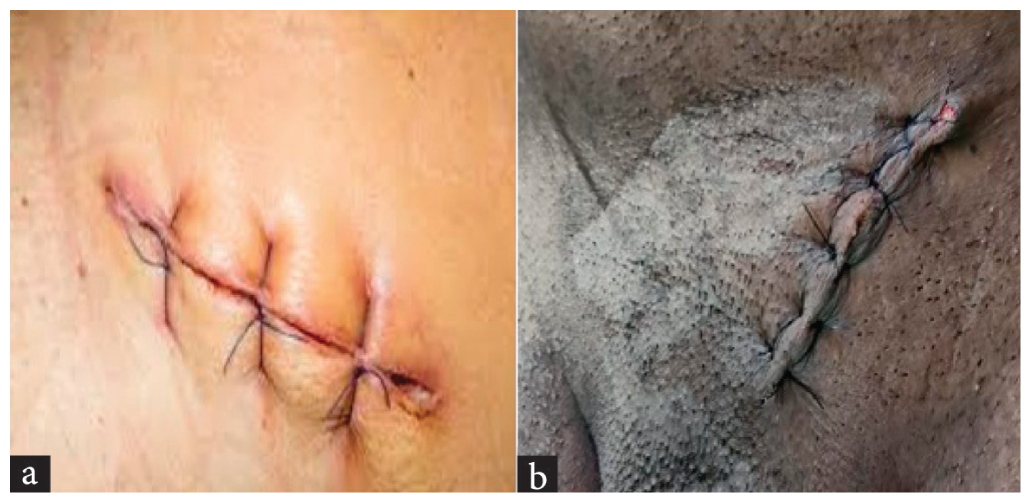
- a) Postoperative image of scalpel, b) Postoperative image of diathermy.
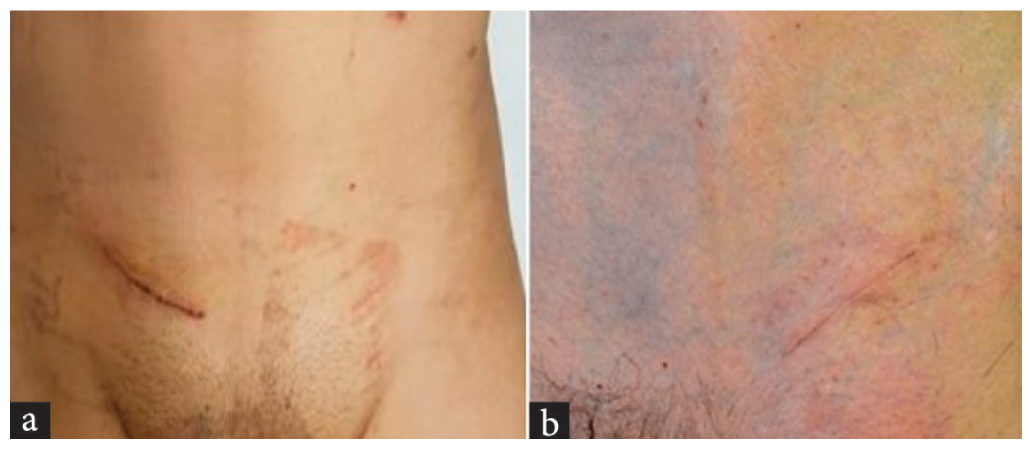
- a) Healed incision after 1 month of Scalpel, b) Healed incision after 1 month of diathermy.
RESULTS
| Male | Female | |
|---|---|---|
| Number | 81 | 0 |
| Diathermy | Scalpel | |
|---|---|---|
| Number | 41 | 40 |
| Age in years | Number |
|---|---|
| 18–25 | 13 |
| 26–35 | 20 |
| 36–45 | 16 |
| 46–55 | 18 |
| 56–65 | 14 |
Mean age of 41.35 ± 1.54 years.
| Diathermy (in sec) | Scalpel (in sec) | P value | |
|---|---|---|---|
| Mean | 4.892± 0.28 | 5.82± 0.24 | <0.0001 |
| SD | 1.74 | 1.603 |
SD- Standard deviation.
| Diathermy (in g) | Scalpel (in g) | P value | |
|---|---|---|---|
| Mean | 2.584± 0.16 | 3.720± 0.19 | <0.0001 |
| SD | 1.04 | 1.26 |
SD- Standard deviation.
| POD-1 | Diathermy (in g) | Scalpel (in g) | P value |
|---|---|---|---|
| Mean | 4.65± 0.12 | 5.45± 0.7 | <0.0001 |
| SD | 0.74 | 0.70 | |
| Median | 5 | 5 | |
| POD-2 | Diathermy (in g) | Scalpel (in g) | P value |
| Mean | 3.92± 0.75 | 4.73± 0.10 | <0.0001 |
| SD | 0.75 | 0.70 | |
| Median | 4 | 5 |
SD- Standard deviation, POD- Post operative day.
| POD-4 | Diathermy (in g) | Scalpel (in g) | P value |
|---|---|---|---|
| Mean | 3.92± 0.32 | 3.76± 0.25 | 0.667 |
| SD | 2.005 | 1.63 | |
| Median | 4 | 3 | |
| POD-10 | Diathermy (in g) | Scalpel (in g) | P value |
| Mean | 2.63± 0.27 | 2.76± 0.25 | 0.727 |
| SD | 1.71 | 1.63 | |
| Median | 2 | 2 | |
| POD-28 | Diathermy (in g) | Scalpel (in g) | P value |
| Mean | 0 | 0.04± 0.04 | 0.228 |
| SD | 0 | 0.30 | |
| Median | 0 | 0 |
SD- Standard deviation, POD- Post operative day.
| POD-4 | Diathermy (in g) | Scalpel (in g) | P value |
|---|---|---|---|
| Mean | 7.73± 0.19 | 8.52± 0.17 | 0.564 |
| SD | 1.22 | 1.13 | |
| Median | 7 | 8 | |
| POD-10 | Diathermy (in g) | Scalpel (in g) | P value |
| Mean | 7.10± 0.11 | 7.904± 0.29 | 0.014 |
| SD | 0.72 | 1.93 | |
| Median | 7 | 7 | |
| POD-28 | Diathermy (in g) | Scalpel (in g) | P value |
| Mean | 5.02± 0.02 | 5.5± 0.17 | 0.008 |
| SD | 0.16 | 1.131 | |
| Median | 5 | 5 |
SD- Standard deviation, POD- Post operative day.
DISCUSSION
Diathermy incisions have historical roots dating back to ancient times and offer several advantages over traditional scalpel incisions, including reduced incision time, lower blood loss, and shorter postoperative recovery. Unlike scalpels, diathermy uses heat to vaporise tissue, creating an incision without spreading heat to adjacent tissues.[9–12]
Electrocautery is considered safe and effective for surgical skin incisions, showing benefits such as faster incision time, reduced blood loss, and lower postoperative pain compared to scalpel incisions. Studies indicate no significant difference in postoperative wound complications, hospital stay duration, or wound cosmetic outcomes between the two techniques.[10,13–17] For instance, a randomised trial revealed that cutting diathermy is the preferred technique for abdominal skin incisions, with no increased risk of wound infection. Additionally, several studies have demonstrated that diathermy incisions result in less postoperative pain.[14,15,18,19]
In elective surgeries, diathermy offers significant benefits over scalpel use, while in emergency surgeries, the results regarding wound healing and complications are more variable. However, the choice between scalpel and diathermy does not significantly impact early postoperative and long-term wound complications, making the decision dependent on the surgeon’s skill and experience.[18–20]
The use of Manchester Scar Score in assessing wound outcomes showed that the mean and median scar scores were slightly higher in scalpel incisions, though the difference was not statistically significant. This aligns with several studies that found no significant difference in scar outcomes between diathermy and scalpel incisions. Further research is needed to fully understand the impact of electrocautery on wound healing and complications.[20–25]
CONCLUSION
Diathermy incision, or electrocautery, is a well-established and effective surgical technique, offering several advantages over traditional scalpel incisions. It reduces procedural time, minimises blood loss, and decreases postoperative pain and complications, making it an attractive option for many surgeries. Our study highlights that diathermy results in less intraoperative blood loss, reduced postoperative pain, and no scar dissimilarity appearance in the techniques, with comparable wound healing outcomes. Diathermy also eliminates the risk of sharp injuries associated with scalpel blades, though precautions must be taken to prevent fire and electrical burns.
However, choosing between diathermy and scalpel depends on factors such as the surgeon’s experience, the specifics of the procedure, diathermy equipment and specifications, and patient considerations. While diathermy offers clear benefits, there are situations where a scalpel may be preferred or necessary. Ultimately, the decision should be based on a careful evaluation of the surgical context and the expertise of the surgical team.
Author contributions
HMA: Study concept, principle investigator, writing the paper; MS: Study concept and writing the paper, co investigator and correction of paper.
Ethical approval
The research/study approved by the Institutional Review Board at Gulbarga institute of Medical Scienece, Gulbarga, number 136/2022-23, dated 18th July 2022.
Declaration of patients consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no Conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
REFERENCES
- The Use of Electrocutting and Electrocoagulation in Surgery. Aust N Zeal J Surg. 1970;39:417-421.
- [CrossRef] [PubMed] [Google Scholar]
- John Marshall’s Sirst Description of Surgical Electrocautery. J R Soc Med. 2011;104:355-360.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Outcome of Skin Incision by Cautery Versus SCALPEL BLADE in Hernia Surgery: A Prospective Cohort Study at a Tertiary Medical College Hospital in South India. Int Sur J. 2017;4:1521-1524.
- [Google Scholar]
- Scalpel Versus Electrosurgery for Abdominal Incisions. Cochrane Database Syst Rev 2012:1-33.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A Study Comparing the Results of Diathermy Incision Versus Scalpel Incision in Patients Undergoing Inguinal Hernioplasty. Indian J Appl Res. 2016;6:555-556.
- [CrossRef] [PubMed] [Google Scholar]
- The Anatomical Basis of Clinical Practice Gray’s Anatomy ((42nd ed.)). 2020.
- A Comparative Study of Scalpel Versus Surgical Diathermy Skin Incisions in Clean and Clean-Contaminated Effective Abdominal Surgeries in AVBRH, Wardha, Maharashtra, India. J Datta Meghe Inst Med Sci Univ. 2017;12:21-25.
- [Google Scholar]
- Diathermy Versus Scalpel Incision in a Heterogeneous Cohort of General Surgery Patients in a Nigerian Teaching Hospital. Niger J Surg. 2015;21:43-47.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Scalpel Versus Diathermy Skin Incision in Caesarean Section. J Obstet Gynaecol. 2019;39:340-344.
- [CrossRef] [PubMed] [Google Scholar]
- Principles of Electrosurgery as Applied to Gynecology. Te Linde’s Operative Gynecology 1997:321-326.
- [Google Scholar]
- Effect of Electrocautery on Wound Healing in Midline Laparotomy Incisions. Am J Surg. 1990;160:618-620.
- [Google Scholar]
- Diathermy vs. Scalpel Skin Incisions in General Surgery: Double-Blind, Randomized, Clinical Trial. World J Surg. 2009;33:1594-1599.
- [CrossRef] [PubMed] [Google Scholar]
- Randomised Controlled Clinical Trial of Scalpel Versus Diathermy for Abdominal Skin Incisions. Indian J Surg. 2021;83:1464-1469.
- [Google Scholar]
- A Comparative Study of Electrocautery Versus Cold Scalpel for Skin Incision in Inguinal Hernia Repair. J Nepalgunj Med Col. 2016;4:14-17.
- [Google Scholar]
- The Visual Analogue Scale: Its Use in Pain Measurement. Rheumatol Int. 1985;5:145-148.
- [CrossRef] [PubMed] [Google Scholar]
- Use of Southampton Scoring for Wound Healing in Post-Surgical Patients: Our Experience in Semi-Urban Setup. Arch Clin Biomed Res. 2021;5:36-41.
- [Google Scholar]
- A Review of Scar Scales and Scar Measuring Devices. Eplasty. 2010;10:e43.
- [PubMed] [PubMed Central] [Google Scholar]
- Electrosurgical Skin Incision Versus Conventional Scalpel: A Prospective Trial. J R Coll Surg Edinb. 1990;35:299-301.
- [PubMed] [Google Scholar]
- Randomized, Clinical Trial on Diathermy and Scalpel Incisions in Elective General Surgery. Iran Red Crescent Med J. 2015;17:e14078.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Outcome of Scalpel Versus Diathermy Skin Incision in Inguinal Hernia Surgery: A Comparative Cross Sectional Study. Birat J Health Sci. 2021;6:1358-1362.
- [Google Scholar]
- Comparison of Electrocautery Incision with Scalpel Incision in Midline Abdominal Surgery – A Double Blind Randomized Controlled Trial. Int J Surg. 2015;19:78-82.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of Superficial Surgical Site Infections Following Use of Diathermy and Scalpel for Making Skin Incisions in Open Inguinal Hernia Repair. Niger J Clin Pract. 2019;12:371-374.
- [Google Scholar]







