Translate this page into:
The Association between Cystitis Cystica and Digital Clubbing: Six Consecutive Cases
*Corresponding author: Priyaranjan Nandy, Department of General Surgery, Command Hospital (EC), Kolkata, India. nandypriyaranjan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nandy P, Prasad A, Madakshira MG, Yegade WS. The Association between Cystitis Cystica and Digital Clubbing: Six Consecutive Cases. Karnataka J Surg. 2025;2:16–20. doi: 10.25259/KJS_2_2024.
Abstract
We report a series of six cases of cystitis cystica confirmed on histopathology, who presented to the urology centre of the tertiary care hospital between September 2023 and July 2024. Clinical examination revealed bilateral digital clubbing of both upper and lower limbs in all cases (Range grade 3 to grade 4). All patients belonged to the male gender aged between 24 years and 43 years. None of them gave a family history of clubbing. Two patients gave a history of having spent time in the high-altitude area (more than 2400 m above sea level) at the time of presentation. None of them displayed cyanosis or any other clinical features of chronic heart or lung diseases. All of them had normal chest X-rays, electrocardiogram, and ultrasonography of the abdomen. The acute phase reactants, biochemical and haematological parameters were within normal limits in all cases. Vascular endothelial growth factor and platelet-derived growth factor may be postulated as the common denominator in the association between clubbing and inflammatory changes in cystitis cystica. The association of cystitis cystica and digital clubbing has not been reported to date. This serendipitous correlation warrants further observation to authenticate the association.
Keywords
Clubbing
Cystoscopy
Histology
Urinary bladder growth
INTRODUCTION
Cystitis cystica is a common benign condition of the urinary bladder with a reactive inflammatory change of the bladder mucosa associated with subepithelial vesicles or cysts formation and glandular metaplasia (cystitis glandularis). Cystitis cystica has been reported to be incidentally detected in 60% of autopsies, with glandular metaplasia seen to affect 2% of the population. Digital clubbing is an important clinical sign characterized by bulbous enlargement of the terminal aspect of the toes and fingers. Clubbing has been traditionally associated with underlying lung or cardiovascular diseases. The association of digital clubbing with cystitis cystica has not been brought out to date. We present a case series of 6 consecutive cases of cystitis cystica who had concomitant digital clubbing, which indicates a possible underlying relationship.
CASE SERIES
Case 1
A 24-year-old male presented in September 2023 with complaints of lower urinary tract symptoms (LUTS), mainly straining and poor urinary stream of six-month duration. He also gave a history of gradually developing polyarthralgia of small joints of the hands over the last two years, which aggravated during winters. He was posted in a high-altitude area and was a non-smoker. Clinical evaluation by a rheumatologist revealed normal acute phase reactants, tender PIP joints, and bilateral grade IV digital clubbing in the upper and lower limbs [Figures 1 and 2]. Ultrasonography showed irregular thickening of the urinary bladder 0.7 × 2.4 × 2.8 cm involving bilateral vesicoureteric junction (VUJ) and mild bilateral hydroureteronephrosis (HDUN). All biochemical parameters, including renal function tests, were within normal limits. Non-contrast computed tomography (CT) of the kidney and urinary bladder revealed endoluminal polypoidal growth at the trigone involving bilateral VUJ, causing mild HDUN. X-ray and CT scan hands showed minimal eccentric periosteal reaction along the lateral surface of the radius and medial surface of the ulnar diaphysis. The chest X-ray was normal. Transurethral resection of the urinary bladder tumour (TURBT) was done along with bilateral double J (DJ) stenting. Histopathological examination (HPE) revealed cystitis cystica and cystitis glandularis. He was also diagnosed him as a case of hypertrophic osteoarthropathy (HOA) and started on non-steroidal anti-inflammatory drugs and bisphosphonates.
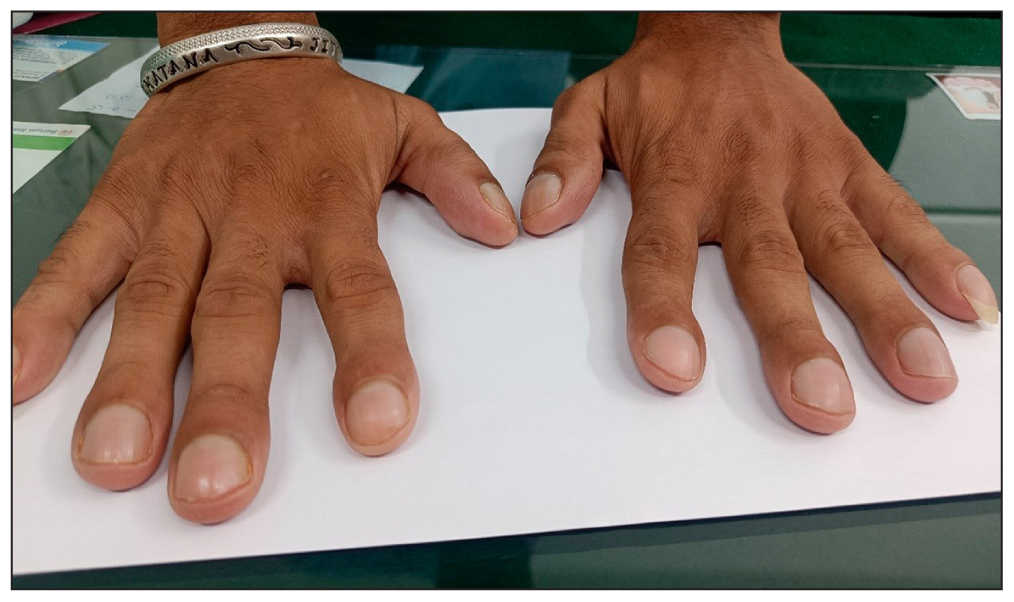
- Advanced bilateral digital clubbing showing bulging and widening of the nail bed.
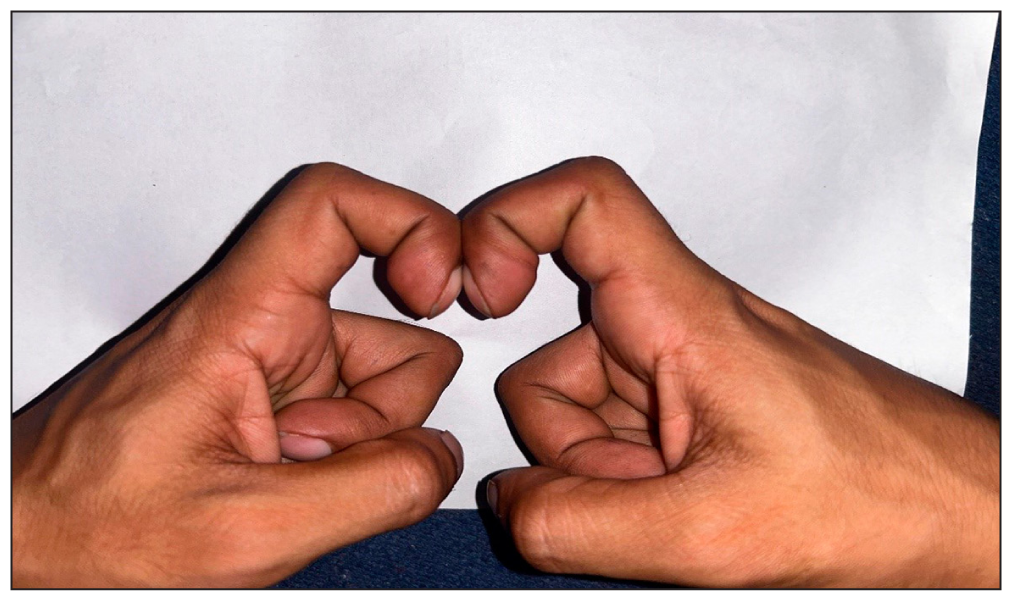
- Schamroth sign elicited by placing the dorsal surfaces of terminal phalanges of corresponding right and left index fingers together.
Case 2
A 33-year-old male, non-smoker, presented in October 2023 with a history of recurrent urinary tract infections for the last six months and recurrent episodes of urinary retention, relieved by repeated catheterization. Clinical examination revealed bilateral grade 3 digital clubbing. Ultrasonography was suggestive of a focal bladder wall irregularly in the trigone area. Cystopanendoscopy (CPE) showed multiple polypoidal growths involving complete trigones and bilateral ureteric orifices. A TURBT, bladder neck dissection, and bilateral DJ stenting were carried out. HPE showed cystitis glandularis.
Case 3
A 43-year-old male smoker and social drinker presented in November 2023 with a history of right flank pain associated with lower urinary symptoms in the form of poor stream for six months. Clinically, no localizing signs were seen except for the presence of grade 4 bilateral digital clubbing. Ultrasonography of the kidney and urinary bladder was suggestive of a space-occupying lesion in the urinary bladder. CT Urography [Figure 3] showed a growth of the posterior-inferior bladder wall extending into bilateral VUJ, causing bilateral mild HDUN. CPE was followed by TURBT, deep muscle biopsy, and bilateral DJ stenting. Histopathology showed cystitis cystitica with cystitis glandularis, and the deep biopsy sent showed normal histology. Check CPE after one month revealed mild oedema around the TURBT site. DJ stents were removed, following which the ureteric orifices were found to be normal.
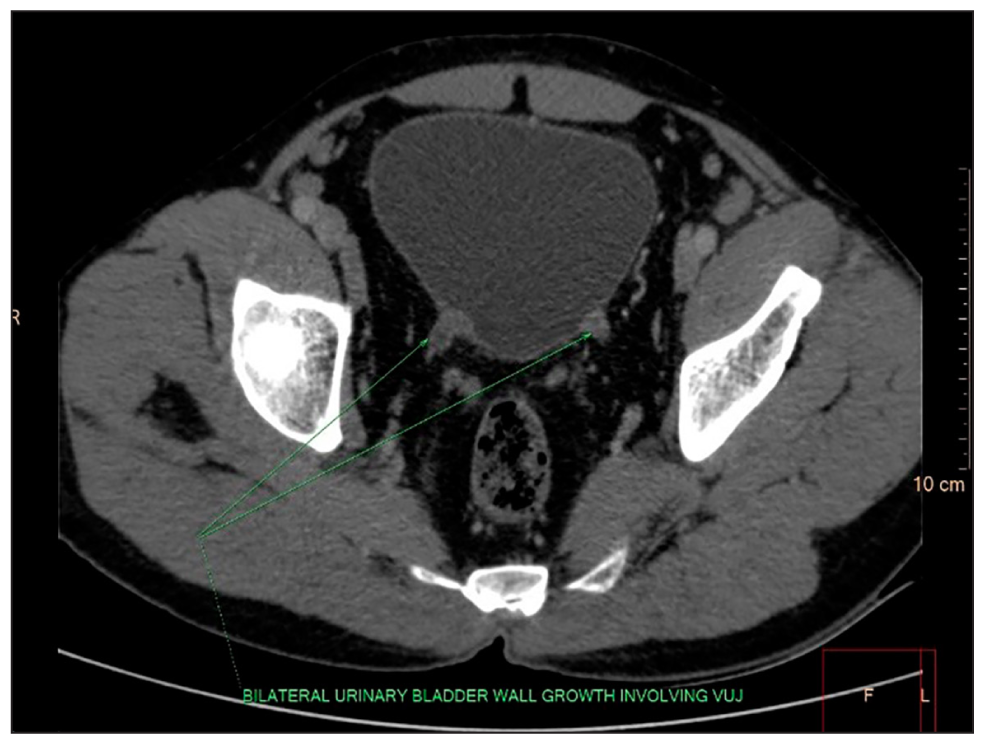
- CT Urography (Post-contast HU:60) Heterogeneously enhancing endoluminal polypoidal wall thickening of the growth of the posteroinferior wall of the bladder with extension into bilateral Vesicoureteric junctions (VUJs). Mild surrounding fat stranding and neovascularisation are seen.
Case 4
A 30-year-old male, nonsmoker, posted in a high-altitude area, presented in November 2023 with a history of burning micturition and occasional haematuria on exertion. Clinically, he had no other localizing signs except for grade 1 clubbing. Urine culture had shown growth of Escherichia coli, for which he was treated with Injection Amikacin. However, his symptoms persisted. CT Urography was done, which showed focal non-enhancing bladder wall thickening over the trigone area. CPE done in November 2023 showed posterior wall thickening with both normal ureteric orifices. A bladder biopsy from the thickened area was reported as cystitis cystica.
Case 5
A 40-year-old male, chronic smoker, and a known case of alcohol dependence syndrome for the last year. Clinical, radiological, haematological, and biochemical parameters revealed no evidence suggestive of hepatic cirrhosis. Routine USG abdomen and pelvis incidentally detected asymmetrical bladder wall thickening of about 6.8 mm, involving both VUJ regions. He had no urinary symptoms. Clinically, he was detected to have bilateral grade 3 clubbing. CT Urography showed a plaque-like minimally enhancing wall thickening of the posterior wall of the urinary bladder adjoining the left VUJ measuring 41 × 9 mm. He underwent CPE [Figure 4], followed by TURBT, and left DJ stenting in May 2024. Per-operative findings showed a bullous edematous growth, which measured 1 × 2 cm on the trigone around the left ureteric orifice. Histopathology of the resected lesion showed cystitis cystica.
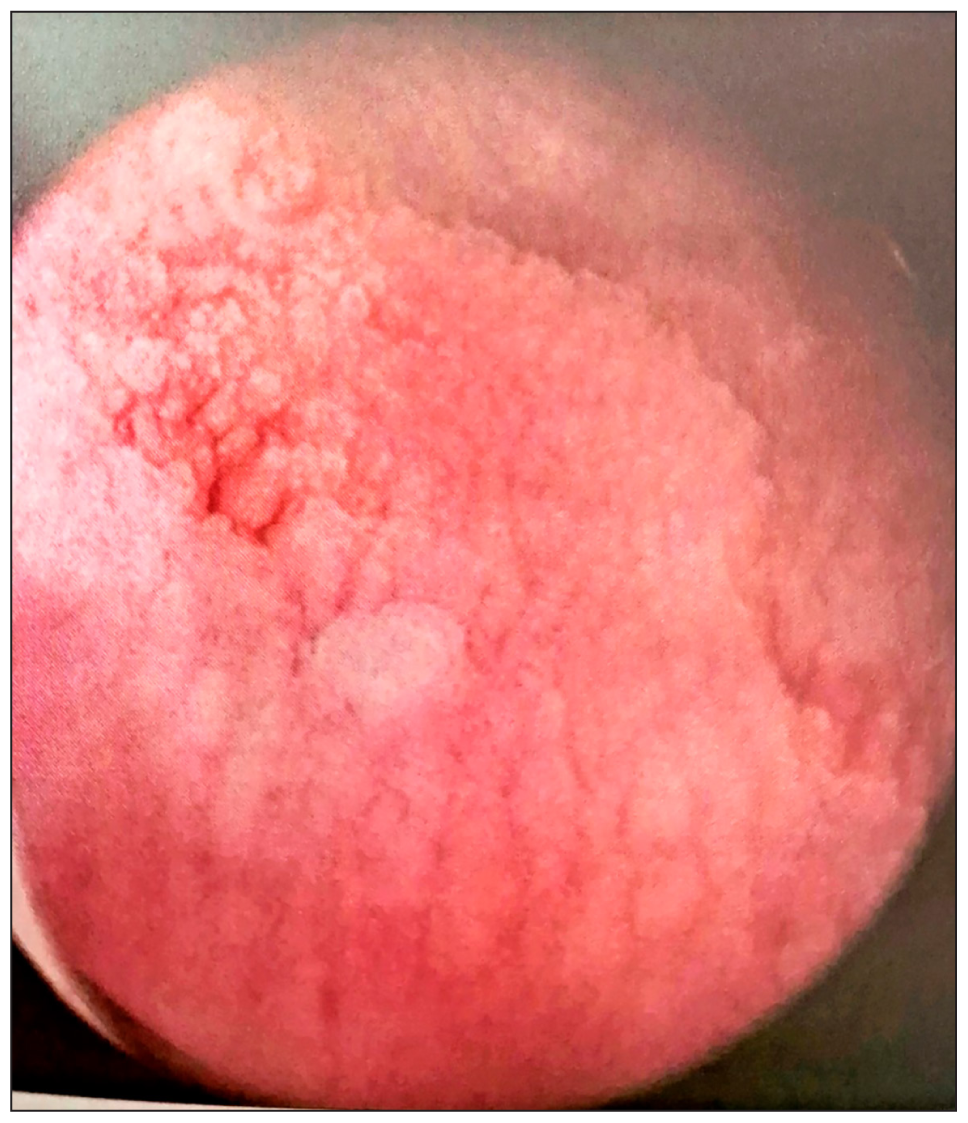
- Plaque in the trigone areas of the bladder, obscuring the left vesico-ureteric junction.
Case 6
A 35-year-old male serving soldier, smoker, and a known case of alcohol dependence syndrome for the last six months. He presented at the medical out-patient department in June 2024 with alcohol withdrawal seizures. Clinical, radiological, haematological, and biochemical parameters revealed no evidence of hepatic cirrhosis. He, however, showed the presence of grade 4 clubbing in bilateral upper limbs. He had no urinary complaints. The USG abdomen incidentally revealed a polypoidal bladder growth around the right VUJ, which measured 12 × 7 mm. All other investigations were within normal limits. He underwent CPE, followed by TURBT and bilateral DJ stenting in July 2024. Per-operative findings revealed diffuse edematous growth near trigone involving both ureteric orifices. Histopathology of the resected tissue showed florid cystitis cystica [Figures 5 and 6].The salient characteristics of the patient have been enumerated in Table 1. All patients had a gradual onset of clubbing, ruling out the possibility of congenital clubbing. The common secondary causes of digital clubbing, such as chronic lung disease, cardiovascular disease, inflammatory bowel disease, malabsorption, and cirrhosis, were excluded with extensive clinical examination and investigations. On follow-up, there was resolution of the bladder lesions with improvement in the LUTS in all the cases. The digital clubbing was persistent in all cases at the time of the last follow-up period.
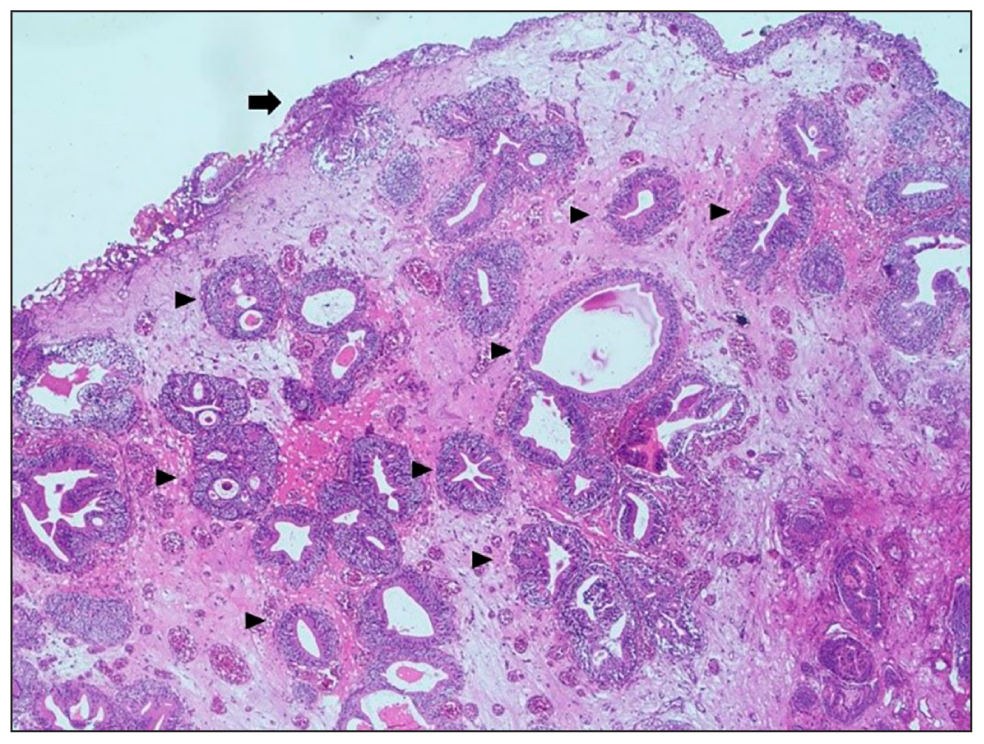
- Haematoxylin and eosin stain (100× magnification) bladder mucosa partially lined by transitional epithelium (arrow) with underlying ingrowth of mucosa in the form of cystitis cystica represented by central space lined by transitional epithelium (arrowheads).
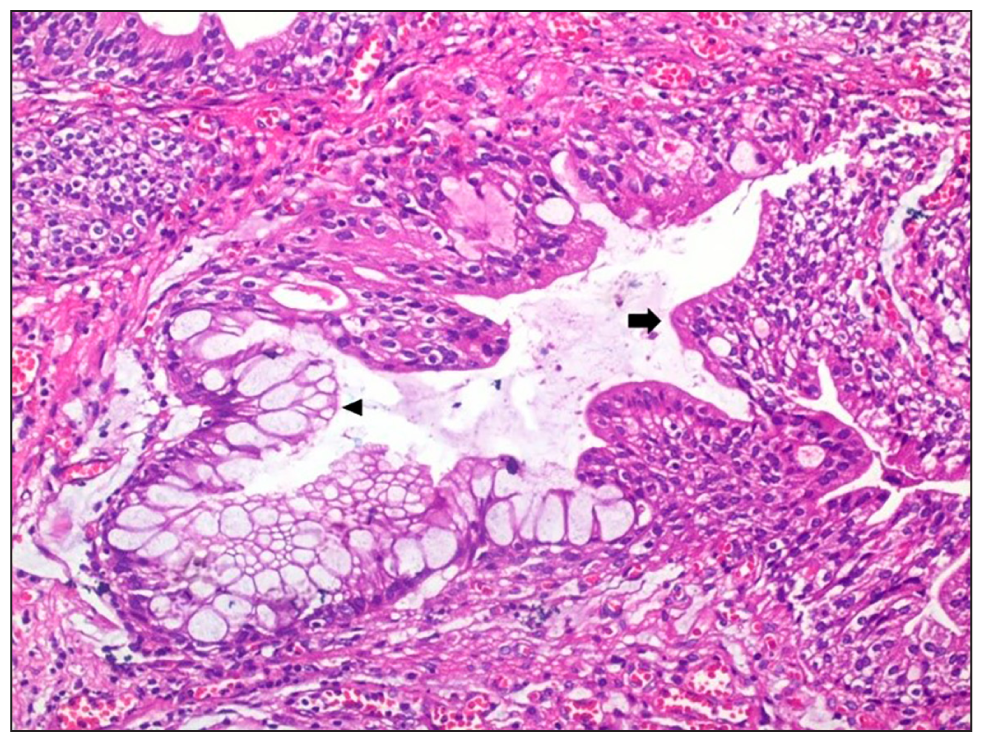
- Haematoxylin and eosin stain (200× magnification) cystitis glandularis is represented by a central space showing partial metaplasia of transitional epithelium (arrow) by mucin-filled goblet cells (arrowhead).
| Case no. | Age (yr) | Duration of onset (months) | Presenting symptom | Smoker (yes/no) | History of stay in high altitude | Grade of cubbing | Imaging | Histopathology |
|---|---|---|---|---|---|---|---|---|
| 1 | 24 | 6 | Straining and poor urinary stream | No | Present | 4 | Irregular thickening of urinary bladder involving bilateral (VUJ) and mild bilateral (HDUN) | Cystitis cystica with cystitis glandularis |
| 2 | 33 | 6 | Recurrent episode of urinary retention | No | Absent | 3 | Focal bladder wall irregularly in trigone area | Cystitis glandularis |
| 3 | 43 | 6 | Right flank pain associated with LUTS and poor stream | Yes | Absent | 4 | Growth of posterior-inferior bladder wall extending into bilateral VUJ with bilateral mild HDUN | Cystitis cystica with cystitis glandularis |
| 4 | 30 | 2 | Burning micturition and ccasional hematuria on exertion | No | Present | 1 | Focal non-enhancing bladder wall thickening over trigone area | Cystitis cystica |
| 5 | 40 | Incidental | No urinary symptom | Yes | Absent | 3 | Asymmetrical bladder wall thickening involving both VUJ region | Cystitis cystica |
| 6 | 35 | 6 | No urinary symptom | Yes | Absent | 4 | Polypoidal bladder growth around right VUJ | Cystitis cystica |
VUJ: Vesicourteric junction, HDUN: Hydroureteronephrosis, LUTS: Lower urinary tract symptoms.
DISCUSSION
Cystitis cystica is typically a benign histopathological lesion associated with the proliferation of Von Brunn nests.[1] The glandular metaplasia of the mucosal cell lining of the bladder is referred to as cystitis cystica et glandularis (CCG). Though CCG and intestinal metaplasia can be related to adenocarcinoma bladder, their relationship is still unclear, and the risk remains low.[2] They often present with LUTS. The risk factors for CCG include chronic UTI, inflammation due to urolithiasis, bladder outflow obstruction, and an indwelling urethral or suprapubic catheter. Treatment involves transurethral resection and relief of obstruction. Although the majority of the cases are innocuous and self-limiting, they may obstruct the ureteral openings and cause renal dysfunction.[3]
Digital clubbing is often associated with certain pulmonary, cardiac, or gastrointestinal disorders that have resulted in reduced oxygen-carrying capacity of blood. Though often asymptomatic, clubbing may predict a sinister underlying disease. It may also present as a hereditary familial anomaly.[4] Primary (idiopathic) clubbing, also called HOA, is hereditary and passed down via genes such as Hydroxy Prostaglandin Dehydronase and SLCO2A1.[5] Vascular Endothelial Growth Factor (VEGF) is a protein that stimulates angiogenesis and is attributed to clubbing.[6] None of our cases had a family history of clubbing. Although the exact pathogenesis of clubbing is not known, the clustering of platelets enhanced by hypoxia releases VEGF and platelet-derived growth factor (PDGF) and has been implicated in the causation.[7] The association between clubbing and cystitis cystica has not been brought out to date except for four cases of digital clubbing, metaplasia of the urinary bladder, and mucous diarrhoea, as observed by Warthin et al.[8] They postulated that factors producing tissue proliferation in the mesodermal structures like bones and digits likewise act on the embryologically similar mesodermal germ cell layer of the bladder trigone and urorectal septum.
The inflammatory process in the urogenital tract can be prompted by causes other than infections. Local mechanical disorders may provoke metaplastic changes of the urothelium or lesions that carry a risk of progression to malignancy.[9] Accumulating evidence suggests that chronic inflammation plays a critical role in the development of urological cancers. Correlations between inflammation and cancer have shown the important role played by hypoxia-inducible factor, as elaborated by Catalino et al.[9] Hypoxic cells secrete angiogenic cytokines, such as VEGF, PDGF, and basic fibroblast growth factor, that stimulate neovascularisation and inflammatory cytokines, such as TNF-α and IL-1β[10]. It is pertinent to consider that VEGF and PDGF could be the common denominators in the association between digital clubbing and inflammatory changes in cystitis cystica. This serendipitous correlation warrants further observation to authenticate the association.
CONCLUSION
This chance association between cystitis cystica and clubbing of hands may be explained by the hypothetical role played by growth factors in a systemic inflammatory milieu and needs further studies for substantiation.
Author contributions
PN and AP: Involved in the surgical management of the cases and drafting the manuscript; YWS: Involved in the medical management of the cases and revising the manuscript; MGM: The histopathological analysis of the biopsies and did the final editing of the manuscript.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
REFERENCES
- A Case of Florid Cystitis Glandularis. Nat Clin Pract Urol. 2007;4:341-5.
- [CrossRef] [PubMed] [Google Scholar]
- Role of Cystitis Cystica et Glandularis and Intestinal Metaplasia in the Development of Bladder Carcinoma. Urology. 2008;71:915-8.
- [CrossRef] [PubMed] [Google Scholar]
- Florid Cystitis Cystica et Glandularis Causing Irreversible Renal Jnjury. Ther Adv Urol. 2021;13:17562872211022465.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Safety and Efficacy of Cyclooxygenase-2 Inhibition for Treatment of Primary Hypertrophic Osteoarthropathy: A Single-Arm Intervention Trial. J Orthop Translat. 2018;18:109-118.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clubbing and Hypertrophic Osteoarthropathy: Insights in Diagnosis, Pathophysiology, and Clinical Significance. Acta Clin Belg. 2016;71:123-30.
- [CrossRef] [PubMed] [Google Scholar]
- Clubbing of Digits, Metaplasia of Urinary Bladder and Mucous Diarrhea. Arch Intern Med (Chic). 1950;86:10-21.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation in Urological Malignancies: The Silent Killer. Int J Mol Sci. 2023;24:866.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Metaplastic Conditions of the Bladder. BJU Int. 2013;112:27-31.
- [CrossRef] [PubMed] [Google Scholar]







